Understanding Joint Replacement
Causes and Treatments Explained
Discover the underlying causes of Joint Replacement and explore effective treatment & management.
Understanding Joint Replacement
The demand for Joint replacement surgeries is increasing due to an aging population and the rising prevalence of arthritis and other joint-related disorders. In 2017, the global number of hip and knee replacements was estimated to be over 2 million annually. By 2025, this number is projected to increase significantly, with knee replacements expected to grow by 673% and hip replacements by 174% compared to 2005 levels.
Joint replacements are more common in older adults – over 60 years of age. However, younger individuals are increasingly undergoing these procedures due to sports injuries and early-onset arthritis.
What is Joint Replacement?
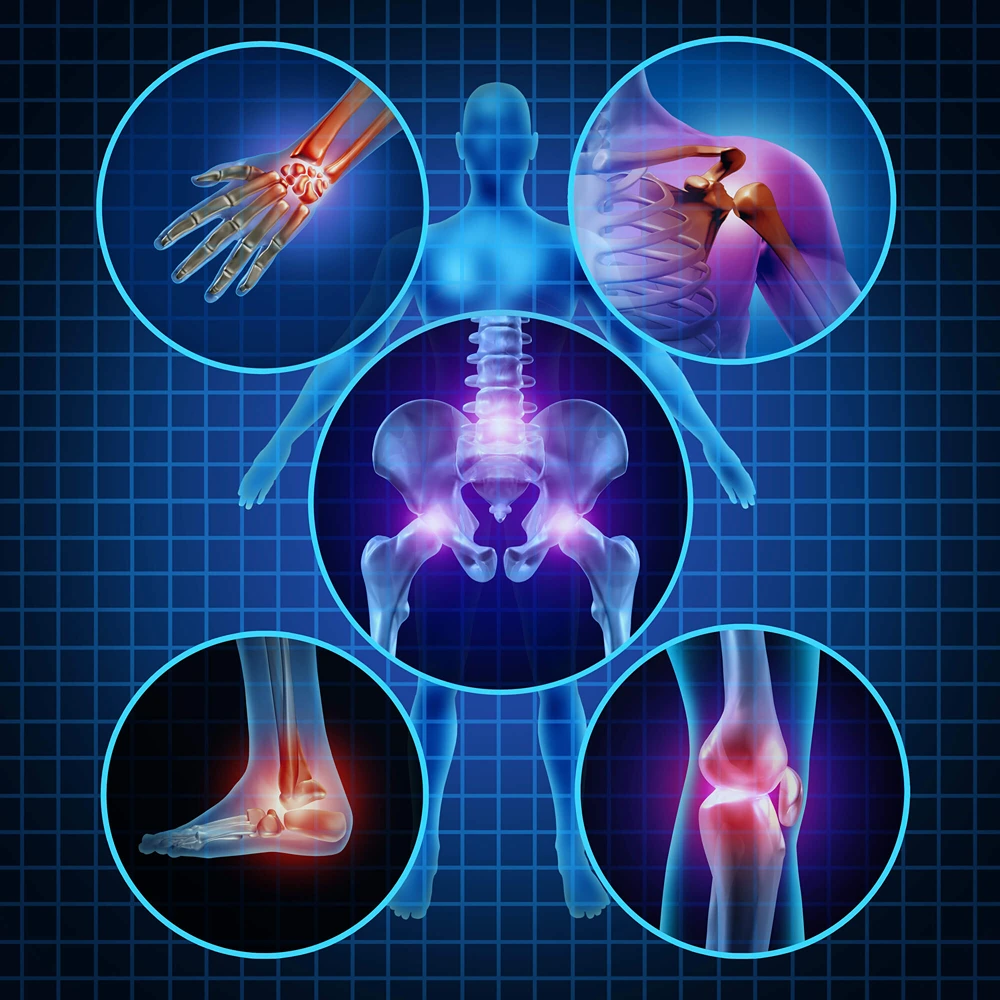
Joint replacement (arthroplasty), is a surgical procedure in which a damaged or diseased joint is removed and replaced with an artificial implant. This procedure is most commonly performed on joints that are heavily used & bear significant weight, such as the hip, knee, & shoulder, but it can also be performed on other joints like the ankle, wrist, & elbow.
Indications for Joint Replacement
Causes Leading to Joint Replacement
Understanding Joint Replacement Health
Risks & Complications of Delaying Joint Replacement Surgery
Delaying joint replacement surgery when it is medically indicated can lead to a variety of risks and complications that can significantly impact a person’s quality of life and overall health.
Here are some of the primary concerns:
- Increased Pain and Discomfort
- Chronic Pain: As joint damage progresses, pain can become more severe and persistent, affecting daily activities and overall well-being.
- Reduced Pain Management Options: Over time, pain may become less responsive to conservative treatments such as medications, physical therapy, and injections.
2. Deterioration of Joint Function
- Decreased Mobility: Progressive joint damage can lead to stiffness and reduced range of motion, making it difficult to perform everyday tasks.
- Loss of Independence: Severe mobility limitations can make it challenging to maintain independence, requiring assistance with personal care and daily activities.
3. Muscle Atrophy and Weakness
- Reduced Physical Activity: Pain and limited joint function can lead to decreased physical activity, causing muscle atrophy and weakness.
- Joint Instability: Weakened muscles around the affected joint can lead to instability and increased risk of falls and injuries.
4. Impact on Mental Health
- Depression and Anxiety: Chronic pain and loss of mobility can contribute to mental health issues such as depression and anxiety.
- Social Isolation: Difficulty participating in social activities and hobbies can lead to feelings of isolation and decreased quality of life.
5. Compensatory Problems in Other Joints
- Overuse of Other Joints: To compensate for the pain and limited function of the affected joint, other joints may be overused, leading to additional pain and damage.
- Secondary Arthritis: Increased strain on other joints can accelerate the development of arthritis in those areas.
6. Development of Severe Deformities
- Joint Deformity: Ongoing joint damage can lead to deformities such as bone spurs and changes in joint alignment.
- Structural Changes: These deformities can make future surgical correction more complex and less effective.
7. Increased Risk of Systemic Health Issues
- Cardiovascular Problems: Limited mobility can contribute to a sedentary lifestyle, increasing the risk of cardiovascular diseases.
- Obesity: Reduced physical activity can lead to weight gain and obesity, which further exacerbates joint problems and overall health.
8. Reduced Effectiveness of Surgery When Finally Performed
- Complicated Surgery: Delaying surgery can make the procedure more complex due to increased joint damage and deformity.
- Longer Recovery Time: Advanced joint damage can lead to a more prolonged and challenging recovery process.
- Suboptimal Outcomes: The longer the delay, the less effective the surgery may be in fully restoring function and alleviating pain.
Delaying joint replacement surgery when it is necessary can lead to severe and wide-ranging complications, including increased pain, reduced mobility, muscle atrophy, mental health issues, compensatory problems in other joints, development of severe deformities, systemic health risks, and reduced effectiveness of surgery when eventually performed. Early intervention is crucial to maintaining quality of life and preventing these negative outcomes.
Types of Joint Replacement
Common Joint Replacement
Getting Prepared for Joint Replacement
Diagnostic Procedures Required Before Joint Replacement
Before undergoing joint replacement surgery, a comprehensive evaluation is necessary to ensure that the procedure is appropriate and to plan for the best possible outcome. The following diagnostic procedures are typically required:
1. Medical History and Physical Examination
- Medical History: A detailed medical history helps identify any underlying conditions that might affect surgery or recovery, such as diabetes, hypertension, or previous joint issues.
- Physical Examination: A thorough physical examination assesses the affected joint’s range of motion, strength, stability, and overall function. It also helps identify any deformities or muscle atrophy.
2. Imaging Studies
- X-rays: X-rays are essential to visualize the extent of joint damage, alignment, and the presence of bone spurs or other deformities.
- Magnetic Resonance Imaging (MRI): MRI scans provide detailed images of the soft tissues, including cartilage, ligaments, and tendons, offering a comprehensive view of joint damage.
- Computed Tomography (CT) Scan: CT scans are used to assess the bone structure in more detail and are particularly useful for complex joint deformities.
3. Blood Tests
- Complete Blood Count (CBC): This test checks for anemia, infection, and overall health status.
- Blood Chemistry Panel: It evaluates kidney and liver function, electrolyte levels, and glucose levels.
- Coagulation Profile: This test assesses the blood’s ability to clot, which is crucial for preventing excessive bleeding during surgery.
4. Cardiovascular Evaluation
- Electrocardiogram (EKG/ECG): An EKG assesses the heart’s electrical activity to identify any abnormalities that might pose a risk during surgery.
- Echocardiogram: This ultrasound test evaluates heart function and can detect any structural heart issues.
- Stress Test: A stress test may be recommended to evaluate cardiovascular health and ensure that the patient can safely undergo anesthesia and surgery.
5. Pulmonary Evaluation
- Pulmonary Function Tests (PFTs): These tests assess lung function to ensure the patient can tolerate anesthesia.
- Chest X-ray: A chest X-ray helps identify any underlying lung conditions, such as chronic obstructive pulmonary disease (COPD) or infections.
6. Infection Screening
- Urine Analysis: This test screens for urinary tract infections that could complicate surgery.
- Nasal Swab: A nasal swab may be performed to check for the presence of MRSA (Methicillin-resistant Staphylococcus aureus), which can cause severe infections.
7. Joint Aspiration (Arthrocentesis)
- Synovial Fluid Analysis: If an infection is suspected or to evaluate inflammatory conditions, a sample of synovial fluid from the affected joint may be analyzed.
8. Preoperative Planning
- Bone Density Test: In patients with osteoporosis or other bone conditions, a bone density test may be conducted to assess bone strength.
- Preoperative Physical Therapy: Evaluating the patient’s current physical condition helps plan preoperative physical therapy to strengthen the muscles around the joint and improve postoperative outcomes.
9. Psychological Evaluation
- Mental Health Assessment: This evaluation helps identify any psychological conditions, such as depression or anxiety, that may affect recovery and adherence to postoperative protocols.
Before joint replacement surgery, a thorough diagnostic process is essential to ensure patient safety and optimize surgical outcomes. This includes medical history and physical examination, imaging studies, blood tests, cardiovascular and pulmonary evaluations, infection screening, joint aspiration, preoperative planning, and psychological evaluation. These assessments help to identify any potential risks and to tailor the surgical and postoperative plan to the patient’s specific needs.
Treatment options for Joint Replacement
Before considering joint replacement, various non-surgical treatments can manage joint pain and improve function. These include medications such as analgesics, NSAIDs, corticosteroids, and DMARDs for rheumatoid arthritis. Physical therapy, through tailored exercise programs and manual therapy, can also be beneficial. Lifestyle modifications like weight management and activity changes, along with assistive devices like braces, supports, canes, and walkers, help stabilize joints and improve mobility.
Surgical Treatment Options
When non-surgical treatments are no longer effective, surgical options are considered. Joint replacement surgery can be total or partial, depending on the extent of joint damage.
Total Joint Replacement (Arthroplasty)
- Knee Replacement: The damaged cartilage and bone are removed and replaced with metal and plastic components.
- Hip Replacement: The damaged hip joint is replaced with a prosthetic ball and socket.
- Shoulder Replacement: The damaged parts of the shoulder joint are replaced with artificial components.
Partial Joint Replacement
- Unicompartmental Knee Replacement: Only the damaged part of the knee is replaced.
- Hemiarthroplasty: Involves replacing only one part of the joint, commonly used in hip fractures.
Revision Joint Replacement
- Performed when a previous joint replacement fails or wears out, requiring a second surgery to replace the old prosthesis with a new one.
Minimally Invasive Joint Replacement
- These techniques involve smaller incisions, potentially reducing recovery time and minimizing tissue damage.
Joint Resurfacing
- Involves reshaping and capping the damaged bone surfaces with metal components, preserving more of the patient’s natural bone.
Arthroscopic Surgery
- A minimally invasive procedure where a small camera and instruments are inserted through tiny incisions to repair joint damage, often used for less severe joint issues.
Treatment options for joint replacement range from non-surgical methods such as medications, physical therapy, lifestyle modifications, and alternative therapies, to surgical procedures like total or partial joint replacement, revision surgeries, minimally invasive techniques, joint resurfacing, and arthroscopic surgery. The choice of treatment depends on the severity of joint damage, patient health, and individual preferences, with the goal of relieving pain, restoring function, and improving the quality of life.
Before considering joint replacement, various non-surgical treatments can manage joint pain and improve function. These include medications such as analgesics, NSAIDs, corticosteroids, and DMARDs for rheumatoid arthritis. Physical therapy, through tailored exercise programs and manual therapy, can also be beneficial. Lifestyle modifications like weight management and activity changes, along with assistive devices like braces, supports, canes, and walkers, help stabilize joints and improve mobility.
Surgical Treatment Options
When non-surgical treatments are no longer effective, surgical options are considered. Joint replacement surgery can be total or partial, depending on the extent of joint damage.
- Total Joint Replacement (Arthroplasty)
- Knee Replacement: The damaged cartilage and bone are removed and replaced with metal and plastic components.
- Hip Replacement: The damaged hip joint is replaced with a prosthetic ball and socket.
- Shoulder Replacement: The damaged parts of the shoulder joint are replaced with artificial components.
- Partial Joint Replacement
- Unicompartmental Knee Replacement: Only the damaged part of the knee is replaced.
- Hemiarthroplasty: Involves replacing only one part of the joint, commonly used in hip fractures.
- Revision Joint Replacement
- Performed when a previous joint replacement fails or wears out, requiring a second surgery to replace the old prosthesis with a new one.
- Minimally Invasive Joint Replacement
- These techniques involve smaller incisions, potentially reducing recovery time and minimizing tissue damage.
- Joint Resurfacing
- Involves reshaping and capping the damaged bone surfaces with metal components, preserving more of the patient’s natural bone.
- Arthroscopic Surgery
- A minimally invasive procedure where a small camera and instruments are inserted through tiny incisions to repair joint damage, often used for less severe joint issues.
Treatment options for joint replacement range from non-surgical methods such as medications, physical therapy, lifestyle modifications, and alternative therapies, to surgical procedures like total or partial joint replacement, revision surgeries, minimally invasive techniques, joint resurfacing, and arthroscopic surgery. The choice of treatment depends on the severity of joint damage, patient health, and individual preferences, with the goal of relieving pain, restoring function, and improving the quality of life.
Get Expert Help Today
Don’t let joint pain hold you back from enjoying life. Contact Max Stone & Surgical Center – Max Hospital Faridabad, for a comprehensive consultation and personalized joint replacement surgery. Our experts team is committed to providing exceptional care & support. Book an appointment to take the first step towards a comfortable & active future.


Get a Call for Appointment
Fill out this form to receive a call from us and schedule your appointment. Start your journey to better health with our expert care today!
