Understanding Piles (Haemorrhoids)
Causes and Treatments Explained
Discover the underlying causes of Piles (Haemorrhoids) and explore effective treatment methods to manage and prevent it.
Understanding Piles (Haemorrhoids)
Piles (haemorrhoids) are a common condition worldwide. They affect people of all ages but are more prevalent in adults aged 45 to 65 years. The exact prevalence varies across regions and populations.
What is Piles (Haemorrhoids)?
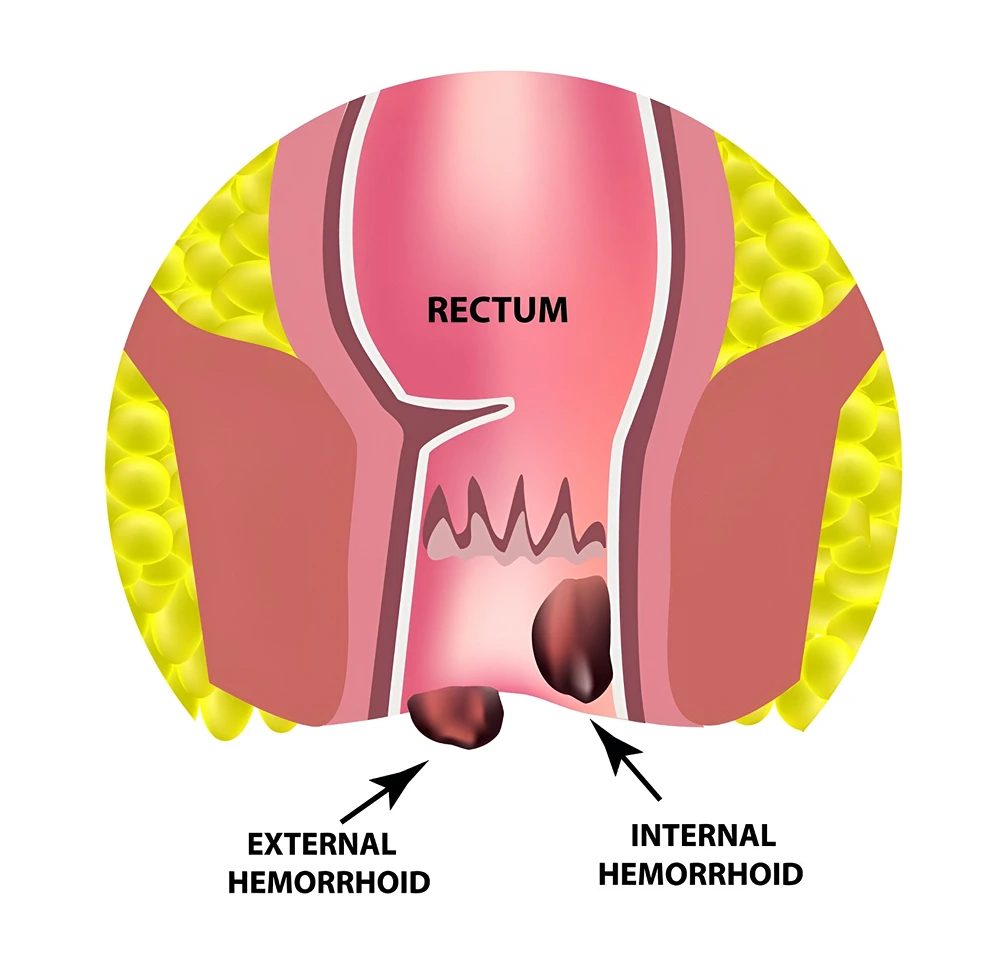
Piles, also known as haemorrhoids, are a prevalent condition affecting both men and women of all ages. They result from prolonged pressure on the veins, often due to factors like constipation, straining during bowel movements, or persistent diarrhea. Genetic predisposition and pregnancy-related pressures on the pelvis can also contribute to their development in women. Lifestyle choices play a significant role as well. For comprehensive information on piles treatment options and various surgical procedures, continue reading this article.
Symptoms of Piles (Haemorrhoids)
Causes of Piles (Haemorrhoids)
Understanding Piles (Haemorrhoids) Health
Risk & Complications of Pile (Haemorrhoids)
-
Bleeding: One of the common complications of piles is bleeding. This can occur during bowel movements when the swollen veins in the rectum or anus are strained or irritated. Blood may appear on toilet paper or in the toilet bowl.
-
Pain and Discomfort: Piles can cause varying degrees of pain and discomfort, especially during bowel movements or when sitting for extended periods. External piles, in particular, can be painful if blood clots form within them (thrombosed piles).
-
Prolapse: In severe cases, internal piles may protrude outside the anus (prolapse) during bowel movements or while sitting. This can lead to difficulty pushing them back in and may require medical intervention.
-
Itching and Irritation: Piles can cause itching and irritation around the anus due to the mucus discharge associated with them.
-
Infection: External piles, especially when thrombosed (containing blood clots), can increase the risk of infection. Symptoms may include increased pain, redness, swelling, and discharge.
-
Strangulation: Occasionally, internal piles can become trapped outside the anus and lose their blood supply (strangulated piles). This is a serious condition requiring immediate medical attention as it can lead to tissue death (necrosis).
-
Anal Fissures: Chronic straining associated with piles can lead to the development of anal fissures (tears in the lining of the anus), which can cause pain and bleeding during bowel movements.
-
Incontinence: Severe cases of piles can affect the anal sphincter muscles, potentially leading to difficulty controlling bowel movements (fecal incontinence).
-
Psychological Impact: Chronic piles can affect quality of life due to pain, discomfort, and embarrassment, impacting daily activities and psychological well-being.
-
Recurrence: Without proper treatment or lifestyle changes, piles can recur or become chronic, requiring ongoing management to prevent complications.
Classification of Piles (Haemorrhoids)
Getting Rid of Piles (Haemorrhoids)
How to Diagnose Piles (Haemorrhoids)
The diagnosis of piles (haemorrhoids) typically involves a combination of medical history review, physical examination, and sometimes additional tests to confirm the presence and severity of the condition. Here’s how it is diagnosed:
- Medical History: The doctor will inquire about your symptoms, including any pain, bleeding during bowel movements, itching, or discomfort in the anal region. They may also ask about your bowel habits and any previous medical conditions related to the digestive system.
- Physical Examination: This involves a visual inspection and a digital rectal examination (DRE). During the DRE, the doctor gently inserts a lubricated, gloved finger into the rectum to feel for any lumps or abnormalities in the anal canal and lower rectum. This helps determine the size, location, and severity of the piles.
- Proctoscopy or Anoscopy: In some cases, the doctor may perform a proctoscopy or anoscopy to directly visualize the inside of the rectum and lower part of the colon. These procedures involve using a thin, flexible tube with a light and camera (proctoscope or anoscope) inserted into the rectum for closer inspection.
- Sigmoidoscopy or Colonoscopy: If internal piles are suspected to be higher up in the rectum or colon, a sigmoidoscopy or colonoscopy may be recommended. These procedures use longer, flexible tubes with cameras to examine the entire colon (colonoscopy) or the lower part of the colon and rectum (sigmoidoscopy). They can help rule out other conditions and assess the extent of the piles.
- Stool Examination: In cases where bleeding is present, a stool sample may be examined to check for the presence of blood and to rule out other gastrointestinal conditions that could cause bleeding.
- Imaging Tests: Occasionally, imaging tests such as ultrasound or MRI may be used to evaluate the anatomy of the anal canal and surrounding tissues, particularly in complex or severe cases.
Treatment of Piles (Haemorrhoids)
The treatment of piles (haemorrhoids) depends on the severity and type of piles, as well as individual patient factors. Here are the common treatment options:
Lifestyle Modifications:
- Dietary Changes: Increasing dietary fiber intake through fruits, vegetables, whole grains, and legumes can soften stools and reduce straining during bowel movements.
- Hydration: Drinking an adequate amount of water helps maintain soft stools and prevents constipation.
- Avoid Straining: Avoiding prolonged sitting on the toilet and straining during bowel movements can help reduce pressure on the veins in the rectal area.
Medications:
- Topical Treatments: Over-the-counter creams, ointments, or suppositories containing hydrocortisone, witch hazel, or numbing agents can help relieve pain, itching, and inflammation.
- Oral Pain Relievers: Non-prescription pain relievers such as acetaminophen or ibuprofen may be used to alleviate discomfort.
Surgical Procedures:
- Hemorrhoidectomy: In severe cases or when other treatments fail, surgical removal of the piles may be necessary. This procedure is performed under general or regional anesthesia.
- Stapled Hemorrhoidopexy (Procedure for Prolapse and Hemorrhoids – PPH): This procedure involves using a circular stapler device to remove excess tissue and reposition the remaining tissue to its normal position.
Minimally Invasive Procedures:
- Transanal Hemorrhoidal Dearterialization (THD): This procedure uses an ultrasound doppler to identify and ligate the blood vessels supplying the piles, reducing their size.
- Laser Treatment: A laser beam is used to remove or shrink the piles, reducing symptoms.
The choice of treatment depends on the severity of symptoms, the type and size of piles, and the patient’s overall health. It’s essential to consult a healthcare provider for proper diagnosis and personalized treatment recommendations.
Get Expert Help Today
Don’t let piles (haemorrhoids) interfere with your life. Contact Max Stone & Surgical Center at Max Hospital Faridabad for a comprehensive consultation and personalized treatment plan. Our experienced team is committed to delivering exceptional care and support. Schedule your appointment today and move towards comfortable future.


Get a Call for Appointment
Fill out this form to receive a call from us and schedule your appointment. Start your journey to better health with our expert care today!
